Is it worth living? Bill Hicks and smoking cessation
They proved that if you quit smoking, it will prolong your life. What they haven’t proved is that a prolonged life is a good thing. I haven’t seen the stats on that yet.
(Bill Hicks, Dark Poet, 1991)
So, you’re a smoker. A committed smoker. And you’re fed up. Fed up of warnings and advice. Fed up of being told what you can do and where you can do it. Most of all, you’re fed up of the offensive assumption that you want to live forever. What matters, you tell yourself, is not the length of your days but the value of each day. And you love smoking. It feels good.
I stopped smoking a long time ago because I was fed up with feeling unhealthy. However, it always annoyed me that people would tell me what to do and act as if I was an idiot. A bit of that annoyance remains. I’m happy not to smoke. It doesn’t feel like I’m missing anything, and life is better now I can jog a bit without falling apart. However, if I didn’t want to get fit, should I have stopped smoking? Similarly, if I didn’t care how long I lived, should I have stopped smoking?
People often complain that public health policy feels invasive, like an assault on our individual right to be as much of a prat as we like as long as it doesn’t directly harm others.
I think there’s a reason it feels invasive, beyond the natural perversity of humanity. Specifically, I think that the problem has three parts:
- We use models to help us make complex decisions, and these have to be simplifications of real life
- When we think about different future events (e.g. thinking about being a non-smoker or being blind), the value we put on that state of being does not match the way we feel when we are actually in it (e.g. actually being a non-smoker or blind). The jargon-y way of saying this is that judgements of utility do not match experienced utility
- Individually, we value losses above gains
The consequence of all this is that what the population rationally prefers may not be what an individual would prefer. More worryingly, it means that what is best for the population, may actually not be best for any individuals.
Don’t worry if you don’t know what I mean…All will (I hope) become clear.
Health states, utility, and how we value life
All models are wrong
When we try to work out the consequences of a new treatment or a new public health policy, we usually produce a model of some sort. These models simulate what would happen to groups of individuals under the new treatment or policy and compare it to what happens at the moment.
To illustrate how these models work, we’ll look at a real one. The diagram below shows the general structure of a model about smoking cessation known as the BENESCO model.
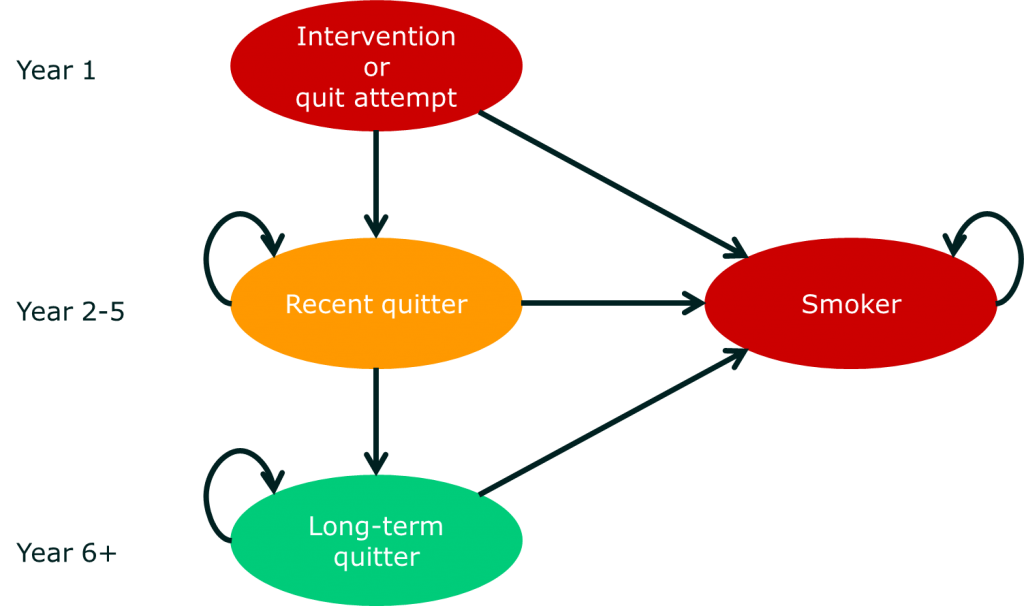 The model starts by looking at a group of people who want to quit smoking. These individuals then either succeed or relapse. In the diagram, each of the ellipses is called a health state. So far, so simple. The complicated bit is what comes next. For each health state, there are a whole series of other health sub-states that relate to different illnesses associated with smoking. The risk of moving into these (disease) sub-states is affected by which of (smoking) states you are in. Here’s the diagram of those sub-states:
The model starts by looking at a group of people who want to quit smoking. These individuals then either succeed or relapse. In the diagram, each of the ellipses is called a health state. So far, so simple. The complicated bit is what comes next. For each health state, there are a whole series of other health sub-states that relate to different illnesses associated with smoking. The risk of moving into these (disease) sub-states is affected by which of (smoking) states you are in. Here’s the diagram of those sub-states:
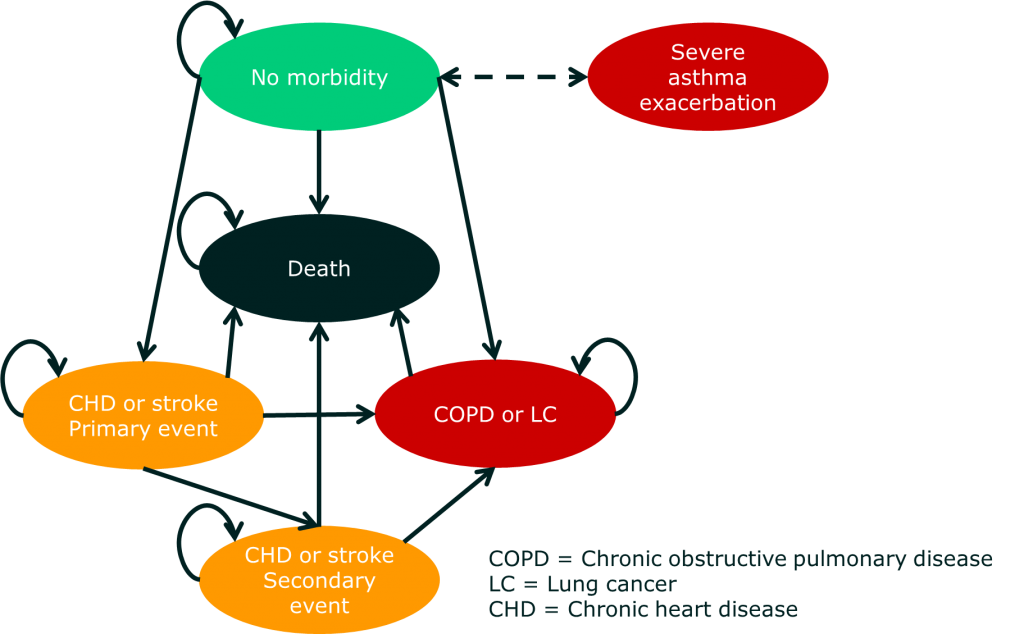 What you may notice is that there are a lot of potential health states that aren’t in the model. Also, all the health states are negative. A lot of smokers would say that they actually enjoy smoking. Indeed, this is part of the reason that smoking cessation models are often restricted to looking at ‘motivated quitters’ (i.e. people who actually want to stop smoking).
What you may notice is that there are a lot of potential health states that aren’t in the model. Also, all the health states are negative. A lot of smokers would say that they actually enjoy smoking. Indeed, this is part of the reason that smoking cessation models are often restricted to looking at ‘motivated quitters’ (i.e. people who actually want to stop smoking).
So, the first reason that Bill Hicks might be unhappy with being told to stop smoking is that the model used to produce recommendations doesn’t include all the various benefits he associates with smoking. Here are some adjustments Bill Hicks might make to the smoking states:
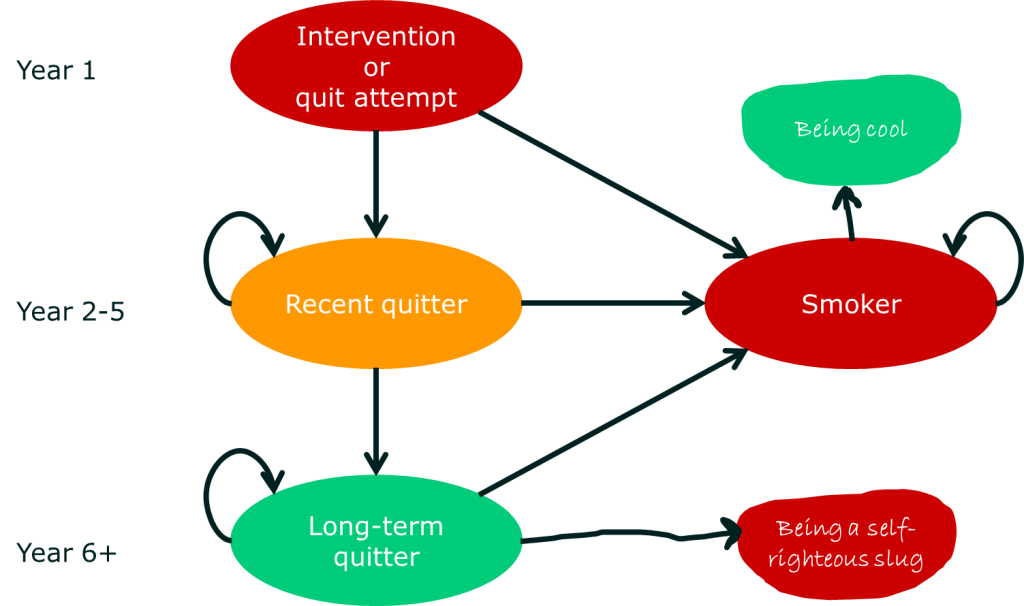 While I don’t see models with the health state ‘Being cool’ getting added to policy decision-making, the point is important. If, as a doctor, you have a patient who really values some state of affairs that is not considered in official policy decisions, you may decide to adjust your advice or at least explain the shortcomings of the guidance.
While I don’t see models with the health state ‘Being cool’ getting added to policy decision-making, the point is important. If, as a doctor, you have a patient who really values some state of affairs that is not considered in official policy decisions, you may decide to adjust your advice or at least explain the shortcomings of the guidance.
Utility and how we value life
The health states in the model are very different from one another. However, in order to make a decision about which treatment or policy to choose, we need to weigh time in all those health states against one another. One approach to doing this is to use utility weights.
Utility refers to the extent to which we value one thing over another based on its ability to satisfy us. In health economics, utility is closely related to the idea of quality of life because we usually judge quality of life on the extent to which people would choose one health state over another.
There’s a big problem in a lot of health economics. When we look at different health states (e.g. smoker, non-smoker, ex-smoker, and lung cancer) we assign utility weights to each health state based on data from the general population.
In the UK, that means that 80% of the people judging the value of being a smoker are non-smokers because 80% of the population do not smoke.
That may sound crazy, but there is a very good reason for this. The general population (in the UK) pays for healthcare, and it is the general population that suffers if funding is not available for hospitals because it is being spent on caring for smokers.
Most of the time, this should not really be a problem. For most health conditions, neither the general public nor the patient wants to be sick. Essentially, we can all agree on the aims of treatment. In the BENESCO smoking cessation model, the smoking states are not really involved in utility calculations, but the disease states are, and no-one (that I know) wants lung cancer.
There are, however, some situations where using the general population to judge utility causes some inconsistency. Here are some examples:
- Chronic disability
Simply put, most of us are horrified by the thought of being physically disabled, but people who have disabilities usually show quite high levels of functional and emotional adaptation. That means that people with disabilities often rate their quality of life more highly than the general population does. Nowhere is this more stark than when looking at issues like euthanasia. A lot of people feel that being paralysed is so bad they would rather die, and yet people with paralysis often report a surprisingly high degree of life satisfaction. Personally, I find this a reassuring testament to the strength of the human spirit, but it does mean that health policy may tend to under-value life spent in a disabled state.
- Addiction
This is really an extension of the same issue as chronic disability. If you are really addicted to a substance, the thought of being without that substance can be horrifying. This is particularly true of addictions associated with severe withdrawal symptoms because addicts may only be able to see the suffering of withdrawal (or the tedium of being sober) and so have a low utility weight for a non-addicted health state. This certainly captures some of the issue with smoking cessation, and may help us understand why it is often a pre-requisite of addiction programmes that the addict wants to be drug-free. I think this captures some of Bill Hicks’ perspective, but not all of it.
- Affective illness
Affective illness is illness that primarily influences our emotions. The main affective illnesses are depression (particularly major depressive disorder), where the predominant mood is depression, and bipolar affective disorder, where mania (heightened or excitable mood) is also present. We all know that, when we are feeling a bit down, our judgement of the value of things can be skewed. Well, the same thing happens when we have clinically severe mood disturbance. And it’s not all one way. As well as the feelings of futility and disinterest that may come with depression, people with mania may feel more positive than is ‘normal’. This has an interesting effect in that it makes utility judgements unreliable. This can be pretty extreme; severe manic episodes may be so intensely pleasurable at the time that individuals would rather be ill than healthy. As a consequence, people acutely ill with affective illness may express utilities (or preferences) for health states that are different to those of the general population. More confusingly, they may express utilities (or preferences) that are different to their utilities at other times. This is a fundamental consideration when psychiatrists are discussing therapies with patients, because there is an issue of whether the patient’s decision while ill should be binding, or whether some guess about what their decision would be at other times needs to be made.
- ‘Self-inflicted’ illness
A lot of illness in Europe, North America, and places like Australia is, at least in part, self-inflicted. In particular, conditions like diabetes, certain types of lung cancer, and liver cirrhosis are generally considered to be largely a result of personal choices about what we eat and drink, and how we look after ourselves. In these situations, our inability to monitor our daily behaviour to avoid long-term health consequences may be, in part, due to various addictions. However, the utility people assign to health states associated with these conditions is probably also, in part, affected by their assessment of this culpability. There is evidence that even primary care staff judge obese patients negatively. Essentially, utility measures for these conditions may include more than just the person’s attitudes towards the health state itself and include bias resulting from judgements about the causes of illness.
All of these examples show that there are a lot of situations in which getting a population estimate of utility, which is used to decide on health policy, may produce estimates that do not reflect patient-experienced utility. In other words, we are making decisions based on beliefs about health that are wrong for individuals. That doesn’t mean they are wrong for the population, of course.
So, the second reason that Bill Hicks might be unhappy with being told to stop smoking is that he doesn’t value health outcomes in the same way as the general population. Specifically, Bill Hicks would probably think that being a smoker is awesome (i.e. has a high utility) but being a non-smoker is boring and hateful (i.e. has a low utility).
Prospect theory and how we hate to lose
Most health economics is based on something called ‘expected utility’. This means that we have a measure for each potential outcome of a health decision based on the assumption that losses and gains have equal value. In the BENESCO model, this means that the utility weight for chronic obstructive pulmonary disease is the same whether you have no illness beforehand or whether you have had a stroke.
Now, imagine you are in normal, good health. That usually has a utility weight of about 0.8. You are offered a drug that has a 60% chance of improving your life to give you perfect health (a utility weight of 1), but there is a 40% chance that it will cause a stroke (utility weight of 0.5).
Whatever happens, your life expectancy remains the same. Would you take the drug?
Now, imagine someone was adding the drug to your water supply. How would you feel about that?
Most people would not take the drug, and most people would be very unhappy to have it added to their water. However, according to expected utility theory, we should be indifferent to whether we take the drug or not. Prospect theory explains how we value the loss of health from stroke more highly than the gain in health from the drug.
The example of adding it to water tells us something about how we, as humans, value our ability to make decisions for ourselves and how this affects the strength of bias we have against losses.
The use of expected utility probably makes sense (though I may well be wrong) when we are looking at population decisions because of the concept of opportunity cost. This means that resources expended on one thing are not available for other purposes. In complex systems involving lots of people, this means that losses for one person are gains (or avoided losses) for others. Working through all the loss aversions in the system would be both incredibly complex (and therefore prone to inconsistency) and may be a waste of time in that all the biases could cancel each other out. There is also the rather more philosophical point that the fact that humans value avoided losses above gains does not mean that it should be the basis of a rational and equitable health system.
The important point, though, is that the use of expected utility means that health economic models are likely to be more relevant on a population level than on an individual level, and so the ‘best’ decision from a population perspective may not be the best decision for an individual. This is particularly important when thinking of public health interventions (such as a ban on smoking in public places) that affect people differentially and result in a small incremental benefit to a lot of people at the cost of (perhaps) a large loss for a smaller number of people.
This gives a third reason that Bill Hicks might be unhappy with being told to stop smoking. If the benefit is felt by someone else, but he experiences the loss, his willingness to accept that loss depends on his belief that the population is more important than the individual. More particularly, it requires him to value the population above himself. I doubt that would sit well with Bill Hicks, and maybe it explains some of the difficulties in nationalised healthcare in the proudly individualistic US.
How should we respond to Bill Hicks?
Of course, Bill Hicks was making a joke, but I do think there’s something important behind it, which boils down to this: health decisions made by insurers, health systems, and even royal colleges are normalised, and humans are anything but normal.
It is (currently) unreasonable and unrealistic to suggest that doctors discussing health with patients should know all the data behind every guideline, personally critique it, and come up with a patient-centred recommendation. What should happen is that the principles underlying these guidelines can be discussed openly so that individuals can make more informed decisions. To return to the quote from the late Bill Hicks:
They proved that if you quit smoking, it will prolong your life. What they haven’t proved is that a prolonged life is a good thing. I haven’t seen the stats on that yet.
we might say:
If you quit smoking, you increase your life expectancy. That may not matter to you, but you will also reduce the amount of time that you are expected to spend with conditions like chronic obstructive pulmonary disease and lung cancer. Most people prefer life spent without those illnesses. Again, you may not, but I doubt it. Therefore, if you quit smoking, the chances are that you will spend more of your life in a state you would like to be in than if you didn’t quit smoking. Of course, life is unpredictable, so there are no guarantees.
This brings us on to the question of communicating just how unpredictable life is to people in a doctor’s surgery. I’ll leave that for another post…

A lively and interesting discussion; well written. I think point 2 – an understanding that there is a disassociation between how you feel now and how you will feel post-intervention is paramount.